Drs. Denise Ferracioli Oda, Roberto Barreto Osaki, Paulo Henrique Weckwerth, Guilherme Ferreira da Silva, Murilo Priori Alcalde, Marco Antonio Hungaro Duarte, and Rodrigo Ricci Vivan discuss a challenging and dangerous condition
Introduction
Infections in the head/neck region present a high level of severity because they are capable of easily dissipating through the fascial spaces and planes of the region.1 When this occurs, the patient could develop Ludwig’s Angina, an extremely fatal clinical condition characterized by a large edema in the neck region that compromises the vital performance of the airways.2
Problems arising from the oral cavity are responsible for 90% of cases of Ludwig’s Angina,3 because the roots of the mandibular teeth are located below the hyoid line of the mandible, which facilitates the dissipation of edema into the submandibular space. However, several other factors can trigger edema in the head and neck area, such as suppurative lymphadenitis, parotiditis, sialolithiasis, and trauma, among others.4 All of these conditions, when unidentified or identified late, may result in dissipation of the edema and its evolution to pneumonia, emphysema, arterial erosion, pericarditis, cardiac arrest, sepsis, and potentially death of the patient.5,6
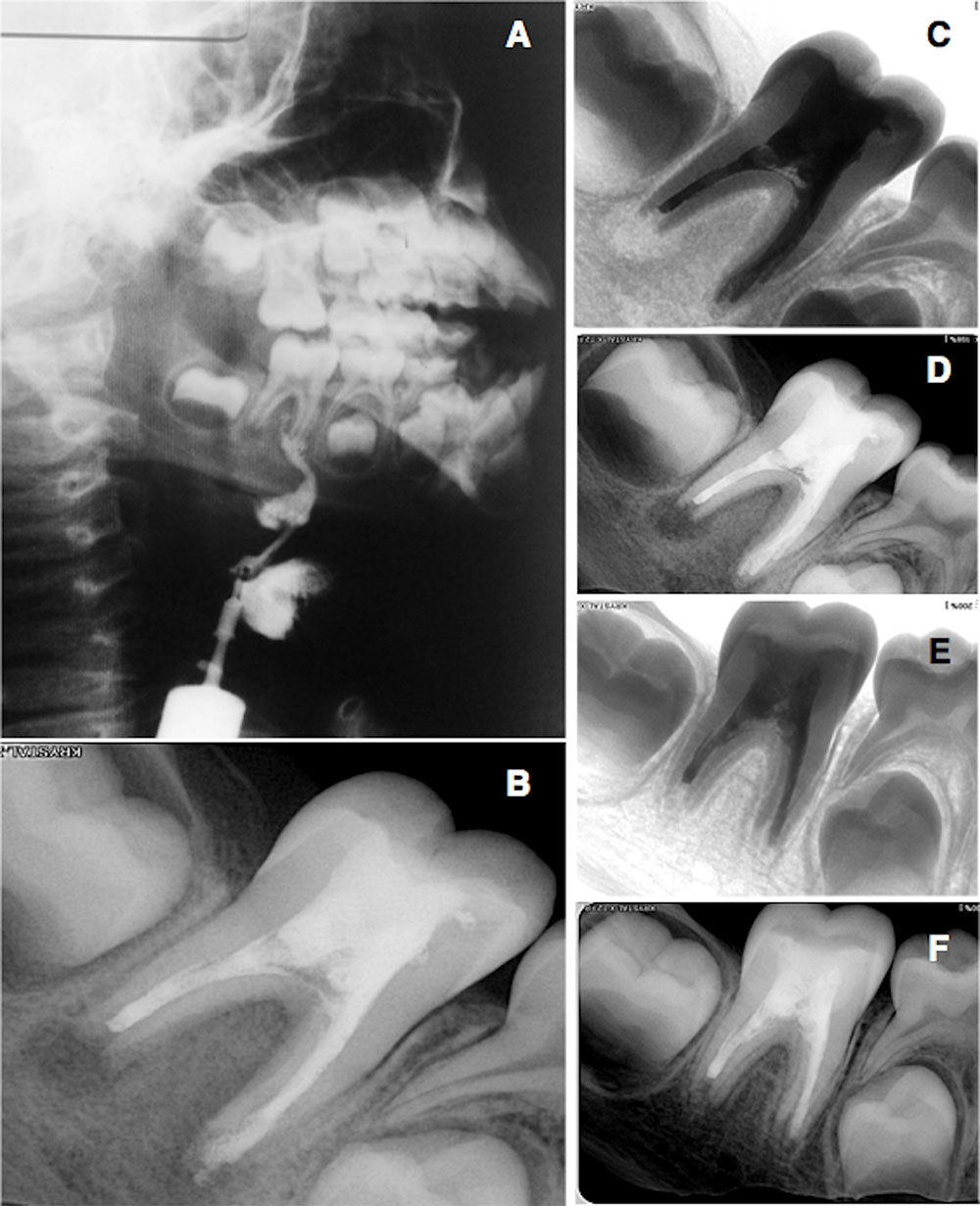
Figures 1A-1F: 1A. Injection of liquid contrast into the extra oral fistula. 1B. Radiographic image of the tooth filled with calcium hydroxide paste added to CMPC, iodoform, and propylene glycol. 1C and 1D. Root canal filling finished. 1E and 1F. control after 6 months
In these cases, complementary exams help in obtaining more precise information about the disease, increasing the chances of an accurate diagnosis. When the intra- or extraoral fistula is present, this may facilitate the investigation because it allows rapid tracking of the cause by injection of contrasts. However, in view of the seriousness of the condition and the rush of emergency procedures, complementary examinations are sometimes omitted, and treatments are performed based on clinical signs only. This underestimation of the disease is serious because it generates long and erroneous treatments, especially if the patient is a child for whom the prognosis becomes more somber.
Thus, it is indispensable for doctors and dental surgeons to collect as much information as possible to prevent fatal complications, enabling them to perform the correct treatment successfully. The present case report described a significant edema in the head and neck region in a 7-year-old child, and provided a description of identifying the cause and performing the treatment of choice.
Case study
The patient, a 7-year-old child, was brought to the dental clinic by his mother, complaining of pain, edema, and an extraoral fistula that had been present for 10 months. Because the fistula was inactive, and the large edema was in the head and neck region, the patient was immediately referred to the hospital for emergency oral drainage. With the suspicion that this infection was of glandular origin, the doctors had scheduled immediate removal of the salivary glands, but the injection of liquid contrast identified the cause as being of dental origin (Figure 1). Therefore, the gland removal surgery was canceled, and after reducing the chances of risk of death, the patient was referred to the dentist.
In the radiographic evaluation, the dentist verified that the origin of the focus of infection was tooth No. 46, which presented pulp necrosis, periapical lesion, and incomplete rhizogenesis at Nolla stage 8. The root canal preparations were performed in the Reciproc® technique with the R25 and R50 instruments (VDW® GmbH, Munich, Germany). During the entire procedure, the canals were irrigated with 2% chlorhexidine solution (Biodinâmica, Ibiporã, PR, Brazil), alternately using saline solution, and the final irrigation was performed with 17% EDTA (Biodinâmica, Ibiporã, PR, Brazil).
The formocresol (Biodinâmica, Ibiporã, PR, Brazil) was used as the first intracanal dressing, and the cavity was sealed with glass ionomer cement (GIC) (Vidrion R, SS White, Rio de Janeiro, RJ, Brazil; Lakewood, New Jersey). After 7 days, the canals were again accessed and irrigated with 2% chlorhexidine and 17% EDTA solutions. They were then completely filled with the second medication, a paste composed of calcium hydroxide powder, camphorated paramonochlorophenol (CPMC) and iodoform (Biodinâmica, Ibiporã, PR, Brazil), all manipulated in propylene glycol (Figure 1). The cavity was again sealed. After waiting 15 days, upon the patient’s return, there was a significant regression of the abscess and fistula, and the patient reported complete cessation of pain and drainage. Thus, the dentist decided to continue with the intracanal medication for another 15 days.
At the end of 30 days with the calcium hydroxide paste medication, complete regression of the abscess was observed, leaving only the scar resulting from extra oral drainage (Figure 2). Before filling the root canals, a hydroxide powder PA (Biodinâmica, Ibiporã, PR, Brazil) plug was inserted in the apical region, and then the root canal filling was performed by the controlled biological technique (Figure 1). After the tooth had been restored, the patient was guided and referred to a plastic surgeon to soften the scar.
The patient did not report pain or any discomfort in final appointment of the treatment. There was total regression of the head/neck edema. In the clinical and radiographic control after 6 months, a regression of the periapical lesion, and biological sealing of the region were observed (Figure 1). During this period, there was continued absence of signs of pain, fistula, and edema (Figure 2).

Figures 2A-2C: 2A. Initial aspect of the fistula in the neck area. 2B. After 30 days. 2C. Final aspect after 6 months
Discussion
Abscesses in the head and neck region are a medical emergency, and the patient should immediately be referred for hospital-level care.4 In the present clinical case report, when the abscess was identified in a critical area, the dental surgeon adopted the correct behavior when requesting immediate medical support to perform the surgical drainage, a protocol indicated in cases of abscess in submandibular space,7 thereby reducing the chances of the patient developing fatal complications.
Complementary exams combined with clinical examination are decisive in identifying the causative agent. However, negligence in the investigation of the disease may result in unnecessary invasive procedures being performed, such as removal of the salivary gland mentioned in the present case. In view of the incorrect diagnosis of sialolithiasis, implementation of the planned procedure would not have favored resolution of the abscess, but would have contributed to the evolution of the infection, and allowed the occurrence of fatal complications, because the true cause would have been identified and treated too late. Only after the injection of contrast was it possible to identify that the cause was of dental origin, tooth No. 46, and the patient was immediately referred to the dental surgeon to begin treatment.
The tooth that caused the infection had incomplete formation of the root apex, a situation that favored the occurrence of injuries to the adjacent periradicular tissues and persistence of the focus of inflammation. In this case, a 2% chlorhexidine solution was used as an irrigating solution during the root canal preparation because it had a low caustic action on the tissues, different from sodium hypochlorite.8 In addition, it exhibited satisfactory antimicrobial action during and after its use. White RR, et al., verified that it continued to exert antimicrobial action up to 72 hours after its use in already instrumented root canals. This effect of chlorhexidine substantivity favored the maintenance of antisepsis and non-recontamination of the root canal.9
The presence of incomplete rhizo-genesis made it difficult to clean the root canal by the mechanical action of the instrumentation and irrigation, so it was essential to use medications in order to overcome this deficiency. The first medication used in this case was formocresol, a substance that has demonstrated absence of genotoxicity by not inducing DNA damage in fibroblasts10 and was capable of promoting high bacterial disinfection in a short period of time,11 helping with stabilization and regression of the infectious focus.
Calcium hydroxide was used as the second intracanal medication to complement disinfection of the root canal. Studies have shown that the addition of camphorated paramonochlorophenol (CMPC) to calcium hydroxide has been able to potentiate its antimicrobial action, and this combination was indicated for procedures of inoculation in infected teeth.12 Studies have shown that the use of this combination in a viscous vehicle further increased the effectiveness and speed of the bactericidal action, in which the paste made with viscous vehicle presented greater antimicrobial efficacy when compared with calcium hydroxide paste only in saline solution.13,14 In addition to the ability to inactivate bacteria and their toxins, calcium hydroxide presented anti-exudative action and ability to induce the formation of mineralized tissue, fundamental properties for the success of the present clinical case.15-17
To prevent periapical tissue injury in teeth with incomplete rhizogenesis, it is necessary to create a physical barrier that allows adequate accommodation of the filling material, without its overflow into the periapical tissues.18 In this case, an apical plug was made with calcium hydroxide powder PA, which not only acted as a physical barrier, but also was biologically tolerated by the organism and had the capacity to induce mineralized tissue formation, characteristics that favored appropriate biological sealing of the apical region.17
Conclusion
The prior and correct identification of the causative agent allowed the adequate treatment in time to avoid the evolution of the disease, preventing the occurrence of fatal complications. The use of different substances and techniques, suitable for the present case, promoted the regression of the focus of infection, in addition to preserving the integrity of the periradicular tissues — fundamental conditions for obtaining posttreatment success.
Acknowledgments
The authors deny any conflicts of interest. The patient’s legal guardian authorized disclosure of the images and information about the case, by means of signing a form of free and informed consent.
- Levitt GW. Cervical fascia and deep neck infections. Laryngoscope. 1970;80(3):409-35.
- Britt JC, Josephson GD, Gross CW. Ludwig’s angina in the pediatric population: report of a case and review of the literature. Int J Pediatr Otorhinolaryngol. 2000;52(1):79-87.
- Tschiassny K. Ludwig’s angina: an anatomic study of the lower molar teeth in its pathogenesis. Arch Otolaryngol. 1943;38(5):485-496.
- Larawin V, Naipao J, Dubey SP. Head and neck space infections. Otolaryngol Head Neck Surg. 2006;135(6):889-893.
- Fritsch DE, Klein DG. Ludwig’s angina. Heart Lung. 1992;21(1):39-46.
- Colmenero Ruiz C, Labajo AD , Yañez Vilas, Paniagua J. Thoracic complications of deeply situated serious neck infections. J Craniomaxillofac Surg. 1993;21(2):76-81.
- Ardehali MM, Jafari M, Hagh AB. Submandibular space abscess: a clinical trial for testing a new technique. Otolaryngol Head Neck Surg. 2012;146(5):716-718.
- Jeansonne MJ, White RR. A comparison of 2.0% chlorhexidine gluconate and 5.25% sodium hypochlorite as antimicrobial endodontic irrigants. J Endod. 1994;20(6):276-278.
- White RR, Hays GL, Janer LR. Residual antimicrobial activity after canal irrigation with chlorhexidine. J Endod. 1997;23(4):229-31.
- Ribeiro DA, Marques ME, Salvadori DM. Lack of genotoxicity of formocresol, paramonochlorophenol, and calcium hydroxide on mammalian cells by comet assay. J Endod. 2004;30(8):593-596.
- Siqueira JF Jr, Rôcas IN, Lopes HP, Magalhães FA, Uzeda M. Elimination of Candida albicans infection of the radicular dentin by intracanal medications. J Endod. 2003;29(8):501–504.
- Frank AL. Therapy for the divergent pulpless tooth by continued apical formation. J Am Dent Assoc. 1966;72(1):87-93.
- Siqueira JF Jr, de Uzeda M. Disinfection by calcium hydroxide pastes of dentinal tubules infected with two obligate and one facultative anaerobic bacteria. J Endod. 1996;22(12):674-676.
- Siqueira JF Jr, Lopes HP, de Uzeda M. Recontamination of coronally unsealed root canals medicated with camphorated paramonochlorophenol or calcium hydroxide pastes after saliva challenge. J Endod. 1998;24(1):11-14.
- Chong BS, Pitt Ford TR. The role of intracanal medication in root canal treatment. Int Endod J. 1992;25(2):97-106.
- Heithersay GS. Calcium hydroxide in the treatment of pulpless teeth with associated pathology. J Br Endod Soc. 1975;8(2):74-93.
- Soares J, Santos S, César C, et al. Calcium hydroxide induced apexification with apical root development: a clinical case report. Int Endod J. 2008;41(8):710-719.
- Holland GR. Periapical response to apical plugs of dentin and calcium hydroxide in ferret canines. J Endod. 1984;10(2):71-74.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..


