 Drs. Francisco Javier Jiménez Enriquez, Jorge Paredes Vieyra, and Fabian Ocampo Acosta discuss the clinical and histopathological findings of periapical inflammatory lesions treated by endodontic surgery
Drs. Francisco Javier Jiménez Enriquez, Jorge Paredes Vieyra, and Fabian Ocampo Acosta discuss the clinical and histopathological findings of periapical inflammatory lesions treated by endodontic surgery
The goal of endodontic treatment is to prevent or cure apical periodontitis (AP) caused by infection of the root canal systems of the affected teeth (Ørstavik and Pitt Ford, 1998) or due to persistence of the primary infection or emergence of infection after treatment (Kuc, Peters, and Pan, 2000). Periapical lesions are the most frequently diagnosed apical odontogenic pathologies in human teeth. The condition is generally described as apical periodontitis. The etiologic factor is the presence and colonization of microorganisms within the pulp canal system (Ørstavik and Pitt Ford, 1998; Kuc, Peters, and Pan, 2000; Nair, et al., 1990). Bacterial stimulus cells cause intercellular mediators, humoral antibodies, and effector molecules to be released into the periapical tissues, as shown by Nair, Henry, and Cano Vera (2005).
When bacteria colonize only in the apical ramifications of the root canal or outside the root canal or when pathosis is sustained by a periapical foreign body, the surgical procedure effectively removes the infected site and enhances the chances of healing (Nair, et al., 1990).
Apical ramifications, lateral canals, and isthmuses connecting main root canals have all been shown to harbor bacterial cells, which are also frequently organized in biofilm-like structures (Nair, Henry, and Cano Vera, 2005; Ricucci, Siqueira, and Bate, 2009; Ricucci, Siqueira, 2010). In their natural habitats, microorganisms almost invariably live as members of metabolically integrated communities commonly attached to surfaces to form biofilms (Costerton, 2007). The biofilm provides microorganisms with a series of advantages and skills, including establishment of a broader habitat range for growth; increased metabolic diversity and efficiency; protection against competing microorganisms, host defenses, antimicrobial agents, and environmental stress; and enhanced pathogenicity (Marsh, 2005).
In situ investigations using optical and/or electron microscopy have allowed observations of bacteria colonizing the root canal system in primary or persistent/secondary infections as sessile biofilms covering the dentinal walls (Nair, 1987; Siqueria, Roças, and Lopes, 2002; Molven, Olsen, and Kerekes, 1991; Carr, Schwartz, Schaudinn, 2009).
Peters, Wesselink, and Moorer reported that poor endodontic treatment allows canal reinfection, which may often lead to treatment failure (1995). Clinical signs and symptoms as well as radiographic evidence of periradicular lesions are usually associated with endodontic failure. When root canal therapy is performed according to accepted clinical principles and under aseptic conditions, the success rate is generally high. The host response is further characterized by bone resorption and an extraradicular infection resulting in radiolucency. An acute apical periodontitis or periapical abscess is associated with clinical signs of inflammation and pain.
Frequent indications for endodontic surgery have been suggested, though contemporary practice proposes that endodontic surgery should be achieved only if conventional endodontic retreatment will not remove potential areas of canal infection such as in an uninstrumented portion of a canal or will have the potential to irreversibly injury the tooth; for example, root fracture following to post removal, or if previous retreatment has not resulted in healing (Love and Firth, 2009).
Apical periodontitis is one of the most common pathological conditions within alveolar bone. Apical periodontitis consists of an inflammation and destruction of the tissues around the root of the teeth caused by etiological agents of endodontic origin (Love and Firth, 2009; Nair, 2006).
It is usually a sequel of an endodontic infection that turns the dental pulp into a necrotic tissue infected by autogenous oral bacteria. This infection usually occurs through dental hard tissue damage resulting from caries, clinical procedures, or trauma, and provokes an inflammatory process that stimulates the proliferation of the cell rests of Malassez in the periodontal ligament, as reported by Nair (2006).
The development of apical periodontitis can occur due to different mechanisms, such as accumulation of osmotic fluid in the lumen, proliferation of epithelial cell rests of Malassez, or molecular mechanisms (Nair, Sjögren, and Sundqvist, 1998).
As a result, clinicians often make clinical and radiographic diagnoses, and the removed periapical tissues are seldom submitted for histopathological analysis (Wang, Cheung, and Ng, 2004). Clinical and radiological evaluations alone cannot properly identify the type of lesion in the apical area (Cotti, et al., 2003; Ricucci, Mannocci, and Ford, 2006).
Sjögren, Hagglund, and Sundqvist report that many factors are involved in the healing process of a periapical defect following endodontic surgery (1990). Among these, the two layers of the periosteum are very important because they may act both as a source of osteocompetent cells and as a barrier against the infiltration of epithelial cells into the healing site. However, in large defects, the periosteum is often damaged by the infective process (Pecora, et al., 2001).
Most persistent lesions remain asymptomatic (Lin, et al., 1991; Salehrabi and Rotstein, 2004; Yu, et al., 2012). Friedman’s study (2002) introduces the concept of asymptomatic function. In addition to the groups “healed,” “healing,” and “non-healed,” the American Association of Endodontists has added the group “functional” to endodontic treatment outcomes (American Association of Endodontists, 2005). The concept of asymptomatic function or functional as a defined treatment outcome has implications for retreatment decision-making. The assumption is that all persistent radiographic lesions represent persistent inflammatory lesions (Brynolf, 1967; 1970).
Matsumato and colleagues showed that the prognosis for the surgical treatment of large periapical lesions was not as good as that of small lesions (Matsumato, et al., 1987). Some authors consider the size of the periapical lesion as a preoperative prognostic factor (Molven, Olsen, and Kerekes, 1991; Wang, Cheung, and Ng, 2004).
The debate
There has been a prolonged debate about the management of large periapical lesions, with some authors suggesting that they can be treated successfully by only surgical means and others proposing that they will heal after nonsurgical root canal treatment (Friedman, 2005).
Periapical surgery attempts to contain any microorganisms within the canal by sealing the canal apically. (At the same time the periapical lesion, if present, can be curetted and histologically investigated.) The objective of this surgical procedure is to optimize the conditions for periapical tissue healing and regeneration of the attachment apparatus.
There are a number of classifications for periapical lesions of endodontic origin based on etiology, symptoms, or histopathological features; for example, the World Health Organization classification leans toward a clinical classification (World Health Organization, 1995).
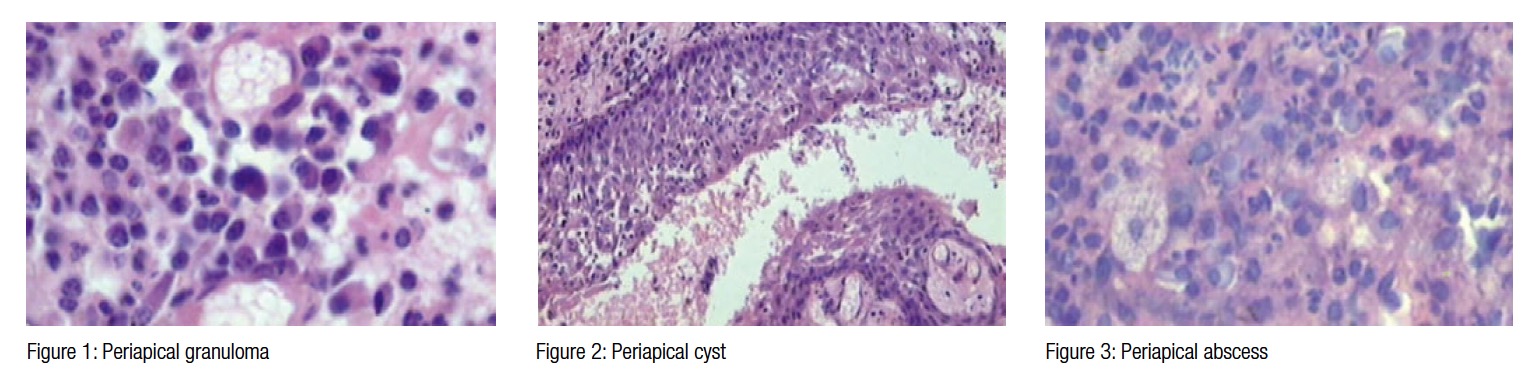
Studies show that a periapical granuloma is the most common periapical lesion of endodontic origin; the diagnosis is based on the presence of connective tissue, blood vessels, and inflammatory cells and may also be called chronic apical periodontitis when chronic inflammatory cells feature or secondary acute apical periodontitis when polymorphonuclear leukocytes are present (Nair, 1997; 2006).
The purpose of the present study was to relate the clinical and histopathological findings of periapical inflammatory lesions treated by endodontic surgery with the results of histopathological investigation of the same lesions.
We hypothesized that the results of histopathological findings related with clinical diagnostic of periapical inflammatory lesions are caused by periapical granulomas.
Material and methods
This study design was an evaluation of a consecutive clinical sample of patients with persistent periapical pathosis who were seen by an endodontist at the University Autonomous of Baja California, School of Dentistry, Tijuana, Mexico. The subjects’ review committee approved the study, and all the participants were treated in accordance with the Helsinki Declaration (World Health Organization, 1996).
A clinical follow-up study was carried out between January 2012 to June 2014; 40 patients with chronic periapical lesions were treated with endodontic surgery after informed consent of each patient had been obtained after explaining the clinical procedures and risks involved and clarifying all questions raised by the patients.
Periapical pathosis was defined as a radiolucent lesion related with a root-filled tooth with either an extending periapical lesion as seen on a radiograph; an unhealed periapical lesion of 5 or more years’ duration post-endodontic treatment (Ørstavik, 1996); or a tooth with a periapical radiolucent lesion with clinical signs and symptoms of periapical pathosis of endodontic origin such as pain, swelling, or sinus tract.
Data were collected using a protocol for each patient and stored in an automated database. The data were coded for later statistical processing.
The inclusion criteria for treatment planning for endodontic surgery were:
- Periapical disease affecting permanent teeth subjected to endodontic treatment, with the presence of pain or inflammation, and repeated failure of root canal treatment
- Periapical disease causing pain or swelling and involving permanent teeth subjected to endodontic treatment with bridge abutments or teeth with posts presenting extraction difficulties
- Where retreatment is impossible owing to fractured instruments, ledges, blockages, and filling material impossible to remove
- An evaluation that any root canal obstacles could not be bypassed or removed to allow full conventional instrumentation of the root canal system.
- With failure of orthograde retreatment where the prognosis of nonsurgical retreatment is unfavorable or impractical (such as an extensive coronal restoration)
- Where biopsy is needed
- Symptomatic gutta-percha over-filling or foreign bodies impossible to remove over an orthograde approach, radiolucencies larger than 8 mm to 10 mm in diameter
Exclusion criteria were patients not meeting inclusion criteria or failure to obtain patients’ authorization. The material for this study consisted of sequential biopsies of roots or root tips together with adhering surrounding apical tissue. Specimens were part of the histologic collection of one of the authors. The material comprised 40 roots from 40 human teeth. Endodontic surgery was not carried out in the acute phase or during exacerbation of a chronic periapical abscess.
Surgical technique
All surgical procedures were carried out by an experienced oral surgeon; endodontic surgery was carried out under local anesthesia. Surgical approach was gained using a complete or partial Newman flaps, and sufficient bone was removed using surgical burs with irrigation to allow curettage of the periapical lesion.
After flap elevation and osteotomy, the periapical lesion and the root end were located. After root-end resection using a fissure bur, the resected root tip and the pathological tissue were curetted out. The intent was to collect the pathological tissue attached to the cut root tip. However, in most cases, the soft tissue and the cut root tip were collected separately.
All patients with clinical findings of acute inflammation such as fistula, swelling, or abscess received antibiotic therapy 2 hours before the surgery (amoxicillin 875 mg with clavulanic acid 125 mg or clindamycin 300 mg in case of penicillin allergy). Strict aseptic conditions were followed to avoid bacterial contamination during surgery.
The periapical lesion was eliminated and placed in formalin (10%). Osteotomy was carried out using round 0.27 mm tungsten-carbide drills (Jota, Switzerland) mounted in a handpiece, and abundant irrigation with sterile physiological saline. The minimum apical resection necessary to access the apex was made, with subsequent apical curettage. The cavity for root-end filling was prepared with ultrasound, Piezon Master (EMS, Electro Medical Systems, Switzerland) and non-diamond ultrasound tips adapted to the different root and anatomic variants.
All other necessary clinical procedures were performed, such as root-end re-section and root-end filling, and the flap sutured. Patients were given standard postoperative instructions and review appointments.
Magnifying glasses of 2.6 magnification Orascoptic™ (Acuity™ System, KaVo Kerr Group) were used to facilitate the procedure. Filling material was introduced and condensed (SuperEBA™, Harry J. Bosworth Company) within the retrograde cavity, in all cases.
Tissue processing
All biopsies were taken during the endodontic surgery and immediately fixed in 10% formaldehyde solution with a surgical specimen/fixator volume ratio of 1:10. Samples were embedded in paraffin using an automated tissue processor (Autotechnicon Processor; Bayer Healthcare, LLC) and then prepared for histopathological diagnosis.
Microtome serial sections (6 to 8 microns) were later made with a Minot rotation microtome (Minotome; IEC). Sections were de-paraffinized and systematically stained with hematoxylin eosin, and a cover slip placed.
The histologic sections were examined under a Bx45 microscope (Olympus, Nishi-Shinjuku, Shinjuku-ku, Tokyo) by two experienced oral pathologists, and a histopathological diagnosis was made as a result by consensus.
The specimens were classified, according to agreed criteria (35) as radicular cyst, scar tissue, or granuloma; it was also highlighted if the granuloma was a mixed form (being classified as epithelized granuloma or granuloma with fibrous tissue).
A diagnosis of periapical granuloma was made based on the histological findings of granulation tissue with inflammatory cells; no distinction was made between the presence of chronic inflammatory cells (chronic apical periodontitis) or acute inflammatory cells (secondary acute periodontitis). A cyst was identified when epithelium was seen to line a lumen, no distinction was made between a true cyst or bay (pocket) cyst; a scar was defined as dense relatively acellular fibrous connective tissue; and an abscess was defined as a collection of pus (dead and dying neutrophils).
Radiographic study
Periapical radiographs were taken before surgery and after 2 years. The images obtained were calibrated (Clini View Version 5.1 program Instrumentarium Imaging, Tuusula, Finland) before being analyzed using the Micro Image Pro®Plus image analyzing system, (Media Cybernetics, Inc.), measuring the area (cm2) of the lesion.
Prognostic assessment healing classification
The following criteria were used to evaluate the success of the periapical surgery. The clinical criteria of Mikkonen and colleagues considering:
- Success — when there is no pain, swelling, or fistula
- Uncertain healing — radiographic evidence of bone destruction and presence or not of symptomatology
- Failure — when there are bone destruction, root resorption, and symptomatology (1983)
The radiographic criteria of Rud, Andreasen, and Jensen (1972):
- Complete healing — complete bone regeneration, normal, or slight increase in width of periodontal periapical space, but less than double the width of the unaffected radicular areas
- Incomplete healing — reduced radiolucency, characterized by signs of bone healing around the periphery of the rarefaction
- Doubtful healing — reduced radiolucency with one or more of the following characteristics: the radiolucency was greater than twice the width of the periodontal space, it was bordered by a structure such as hard lamina, it had a circular or semi-circular periphery, or was located symmetrically “cone-like” around the apex as an extension of the periodontal space
- Radiographic failure — there were no changes, or there was an increase in radiolucency (1972)
The clinical and radiographical criteria of Von Arx and Kurt to determine overall evolution:
- Success — when bone regeneration was ≥90% and the pain and clinical scales were 0 (on a scale of 0 to 3)
- Improvement – when bone regeneration was between 50% and 90%, and the pain and clinical scales were 0
- Failure – when bone regeneration was less than 50%, or there were clinical symptoms (1999)
Finally, it was evaluated if the tooth was functional (remained in place) or not (Friedman, 2003).
Statistical analysis
The data were coded for later statistical processing using the SPSS version 20 for Windows. Descriptive statistics were calculated for the relevant variables; specifically, means, maximum, and minimum relationships were studied using analysis of variance (ANOVA) with subsequent Tukey testing and calculation of Pearson’s correlation coefficient. The hypothesis tests were conducted at the 0.05 level of significance.
Results
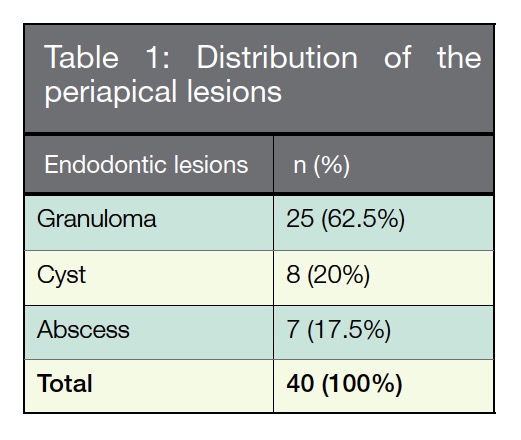
The study comprised 40 patients, 26 women (65%), and 14 men (35%) at a mean age of 43.54 years (range, 18 to 69 years) with 40 biopsy samples (Table 1). The outcomes demonstrated that 40 cases were sent to the Laboratory of Oral Pathology, Facultad de Odontología Tijuana with a clinical diagnosis of periapical inflammatory lesions. A possible diagnosis of periapical granuloma was hypothesized, after the histopathological analysis (Table 1); all cases were diagnosed as Granuloma (62.5%), Cyst (20%) and Abscess (17.5%).
Our results showed that UR2 had a high percentage of periapical lesion corresponding to periapical granuloma associated with overfilled canals (Table 1).
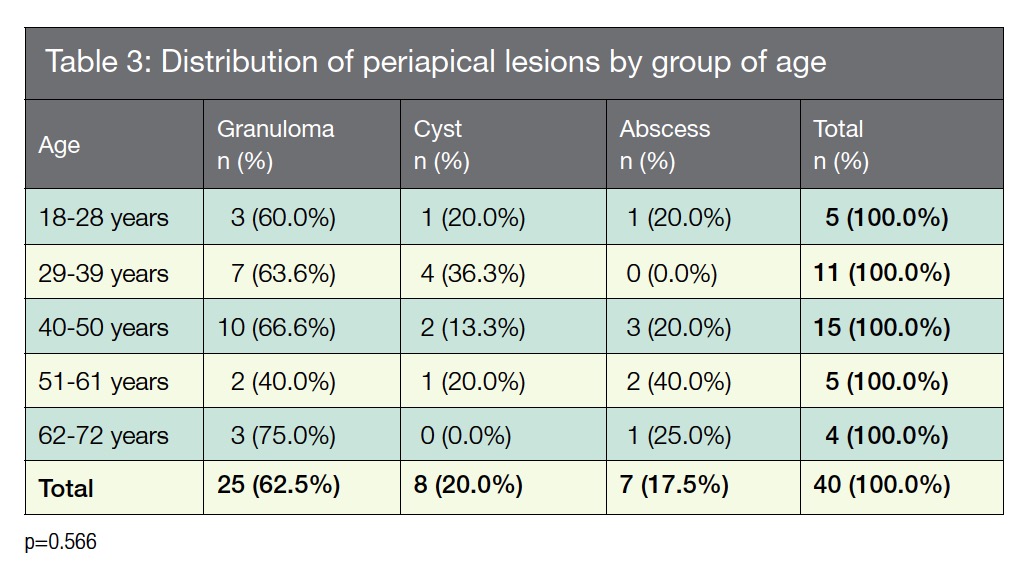
The distribution of periapical lesions by age (Table 3) were high in patients with 40-50 years old with diagnostic of granuloma (66.6%).
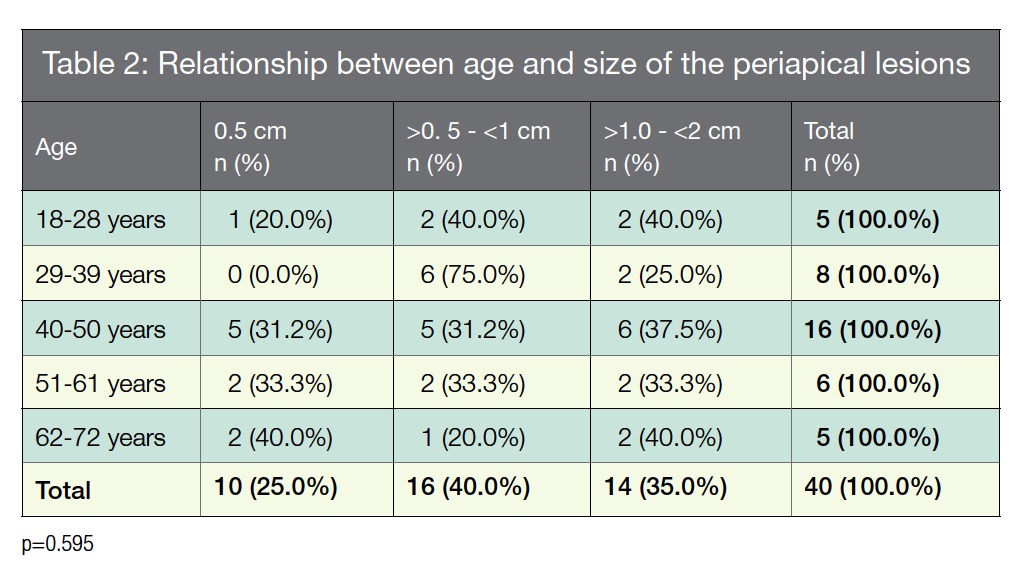
 According to the lesion’s size and patient’s age (Table 2 and 3), these were identified as periapical Granulomas in the group of 40-50 years of age (66.6%) with a size of >1.0 – <2 cm (37.5%).
According to the lesion’s size and patient’s age (Table 2 and 3), these were identified as periapical Granulomas in the group of 40-50 years of age (66.6%) with a size of >1.0 – <2 cm (37.5%).
There was no difference between men and women, and the fourth and fifth decades of life were the most affected (Table 3).
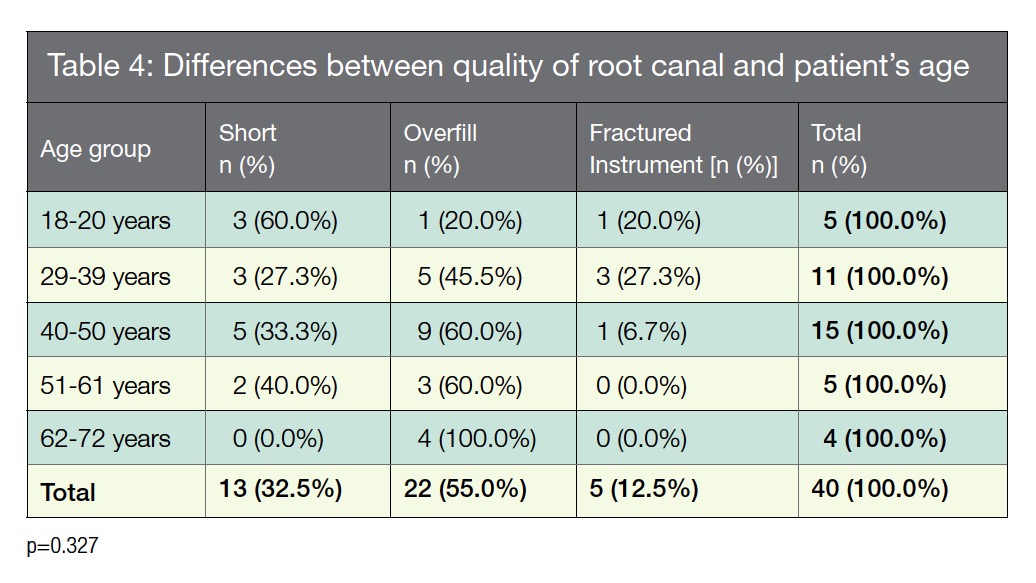
Relation between age and the quality of the root canal treatment showed no statistical relevance (Table 4).
Discussion
The most common periapical lesions of endodontic origins are periapical abscess, granuloma, and cysts (Figures 1-3), all these periapical pathoses, with different treatment and prognostic implications considered clinically suggestive of apical periodontitis, and they must be confirmed by histopathological examination (Gulabivala and Briggs, 1992; Nohl and Gulabivala, 1996).
 Because microorganisms are the essential etiological agents of primary apical periodontitis (Kakehashi, Stanley, and Fitzgerald, 1965) and also the major cause of posttreatment apical periodontitis (Nair, et al., 1990; Molander, et al., 1998; Siqueira and Rôças, 2004), the cherished goal of treatment of the disease has been a total elimination of the intraradicular infection and prevention of reinfection.
Because microorganisms are the essential etiological agents of primary apical periodontitis (Kakehashi, Stanley, and Fitzgerald, 1965) and also the major cause of posttreatment apical periodontitis (Nair, et al., 1990; Molander, et al., 1998; Siqueira and Rôças, 2004), the cherished goal of treatment of the disease has been a total elimination of the intraradicular infection and prevention of reinfection.
These observations are fully in accordance with similar findings reported before by Sundqvist and colleagues (1998). According with Pellegrino, patients with posttreatment apical periodontitis are faced with contrasting alternatives, including nonsurgical or surgical management intended to cure and retain the affected tooth (Pellegrino, 1994).
All the samples examined in the present study were obtained during endodontic surgery by the first authors using strict clinical inclusion and exclusion parameters from teeth with persistent apical pathology.
The incidence of periapical cysts among periapical lesions varies from 6% (Block, 1976) to 55% (Priebe, Lazansky, and Wuehrmann, 1954). In the present study, more than half of the periapical lesions analyzed had a final diagnosis of periapical granuloma cyst (53%), and periapical cyst represented 20% (n=8) of the cases.
This study did not examine the cystic lesions to determine whether they were a true cyst or a bay/periapical pocket cyst because in the majority of cases root apices were not included in the biopsy material, and the material often was not able to be removed in total. As such, a true representation of the type of cyst could not be reliably made (Nair, 1998).
Matsumato and colleagues reported that the prognosis for the treatment of large periapical lesions was not as good as that of small lesions (1987). Harrison and Juroski (1992) state that if the lesion is small, then all the pathologic tissue can easily be removed; however, if the lesion is large, then it is more likely that curettage will be incomplete and thus unsuccessful.
On the other hand, Rahbaran, Gilthorpe, and Harrison suggest that the lesion size has no significant influence on the success of treatment (2001). Likewise, Strindberg (1956) and Sjögren and colleagues (1990) found no significant differences in healing frequency between lesions initially larger or smaller than 5 mm.
It is clear that the prognosis for a periapical lesion depends on its origin, type, and radiographic size, and the ultimate success of endodontic surgery is dependent on a myriad of factors. These include the quality of the orthograde root canal filling, the apical root-end filling, size of the periapical destruction, experience of the operator, the type of periapical pathology, use of antibiotics, status of the coronal restoration, and the method of preparing the apical root-end cavity (Carr, 1992; Maddalone and Gagliani, 2003).
The patient’s systemic condition to the history of the individual teeth, case selection, surgical materials, and techniques, and the surgeon’s interpretation of the short and long-term clinical and radiographic findings are other points to consider (Gutmann and Harrison, 1991).
An accurate histopathological diagnosis was only possible when the lesion was removed as a whole, and if a serial sectioning or step-serial sectioning was performed. According to Nair and colleagues, this is possible because in a routine histological report, the presence of an epithelialized lesion is reported as a radicular cyst, but often this report is inappropriate (1996).
Conclusion
The outcomes of the present study show a high number of periapical granulomas among periapical cysts and confirms that periapical granulomas and cysts are the most common periapical lesions of endodontic origin associated with persistent periapical pathosis.
However, other studies have shown a different perspective in the diagnosis of periapical cysts, and more prospective studies are necessary for better clarification of these data. Moreover, this study highlights the importance of the histopathological evaluation for a proper diagnosis of periapical pathosis.
References
- American Association of Endodontists. Approved definitions of endodontic outcome. Colleagues for Excellence. Chicago, IL: 2005.
- Block RM, Bushell A, Rodrigues H, Langeland K. A histopathologic, histobacteriologic, and radiographic study of periapical endodontic surgical specimens. Oral Surg Oral Med Oral Pathol. 1976;42(5):656-678.
- Brynolf I. A histological and roentgenological study of the periapical region of human upper incisors. Odonto Revy. 1967;18(suppl 11):1-176.
- Brynolf I. Roentgenologic periapical diagnosis. II. One, two or more roentgenograms? Sven Tandlak Tidskr. 1970;63(5):345-350.
- Carr GB. Microscopes in endodontics. J Calif Dent Assoc. 1992;20(11):55-61.
- Carr GB, Schwartz RS, Schaudinn C, Gorur A, Costerton JW. Ultrastructural examination of failed molar retreatment with secondary apical periodontitis: an examination of endodontic
biofilms in an endodontic retreatment failure. J Endod. 2005;35(9):1303-1309. - Costerton JW . The Biofilm Primer. Berlin: Springer-Verlag Berlin Heidelberg; 2007.
- Cotti E, Campisi G, Ambu R, Dettori C. Ultrasound real-time imaging in the differential diagnosis of periapical lesions. Int Endod J. 2003;36(8):556-563.
- Friedman S. Prognosis of initial endodontic therapy. Endod Topics. 2002;2:59-88.
- Friedman S. Etiological factors in endodontic post-treatment disease: apical periodontitis associated with root filled teeth. Endod Topics. 2003;6:1-2.
- Friedman S. The prognosis and expected outcome of apical surgery. Endod Topics. 2005;11(1):219-262.
- Gulabivala K, Briggs PF. Diagnostic dilemma: an unusual presentation of an infected nasopalatine duct cyst. Int Endod J. 1992;25(2):107-111.
- Gutmann JL, Harrison JW. Surgical Endodontics. Boston, MA: Blackwell Scientific Publications; 1991: 338-384.
- Harrison JW, Jurosky KA. Wound healing in the tissues of the periodontium following periradicular surgery. III. The osseous excisional wound. J Endod. 1992;18(2):76-81.
- Kakehashi S, Stanley HR, Fitzgerald RJ. The effects of surgical exposures of dental pulps in germfree and conventional laboratory rats. Oral Surg Oral Med Oral Pathol. 1965;20:340-349.
- Kuc I, Peters E, Pan J. Comparison of clinical and histologic diagnoses in periapical lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89(3):333-337.
- Lin LM, Pascon EA, Skribner J, Gängler P, Langeland K. Clinical, radiographic, and histologic study of endodontic treatment failures. Oral Surg Oral Med Oral Pathol. 1991;71(5):603-611.
- Love RM, Firth N. Histopathological profile of surgically removed persistent periapical radiolucent lesions of endodontic origin. Int Endod J. 2009;42(3):198-202.
- Maddalone M, Gagliani M. Periapical endodontic surgery: a 3-year follow-up study. Int Endod J. 2003;36(3):193-198.
- Marsh PD. Dental plaque: biological significance of a biofilm and community life-style. J Clin Periodontol. 2005;32(suppl 6):7-15.
- Matsumoto T, Nagai T, Ida K, Ito M, Kawai Y, Horiba N, Sato R, Nakamura H. Factors affecting successful prognosis of root canal treatment. J Endod. 1987;13(5):239-242.
- Mikkonen M, Kullaa-Mikkonen A, Kotilainen R. Clinical and radiologic re-examination of apicoectomized teeth. Oral Surg Oral Med Oral Pathol. 1983;55(3):302-306.
- Molander A, Reit C, Dahlén G, Kvist T. Microbiological status of root-filled teeth with apical periodontitis. Int Endod J. 1998;31(1):1-7
- Molven O, Olsen I, Kerekes K. Scanning electron microscopy of bacteria in the apical part of root canals in permanent teeth with periapical lesions. Endod Dent Traumatol. 1991;7(5):226-229.
- Molven O, Olsen I, Kerekes K. Scanning electron microscopy of bacteria in the apical part of root canals in permanent teeth with periapical lesions. Endod Dent Traumatol. 1991;7(5):226-229.
- Nair PN, Henry S, Cano V, Vera J. Microbial status of apical root canal system of human mandibular first molars with primary apical periodontitis after ‘‘one-visit’’ endodontic treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99(2):231-252.
- Nair PN, Sjögren U, Krey G, Sundqvist G.Therapy-resistant foreign body giant cell granuloma at the periapex of a root-filled human tooth. J Endod. 1990;16(12):589-595.
- Nair PNR. Light and electron microscopic studies of root canal flora and periapical lesions. J Endod. 1987;13(1):29-39.
- Nair PN. Apical periodontitis: a dynamic encounter between root canal infection and host response. Periodontol 2000. 1997;13:121-148.
- Nair PN. New perspectives on radicular cysts: do they heal? Int Endod J. 1998;31(3):155-160.
- Nair PN. On the causes of persistent apical periodontitis: a review. Int Endod J. 2006;39(4):249-281.
- Nair PNR, Pajarola G, Schroeder HE. Types and incidence of human periapical lesions obtained with extracted teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81(1):93-102.
- Nair PNR, Sjögren U, Kahnberg KE, Krey G, Sundqvist G. Intraradicular bacteria and fungi in root-filled, asymptomatic human teeth with therapy-resistant periapical lesions: a longterm
light and electron microscopic follow-up study. J Endod. 1990;16(12):580-588. - Nair PN, Sjögren U, Sundqvist G. Cholesterol crystals as an etiological factor in non-resolving chronic inflammation: an experimental study in guinea pigs. Eur J Oral Sci. 1998;106(2pt 1);644-650.
- Nohl FS, Gulabivala K. Odontogenic keratocyst as periradicular radiolucency in the anterior mandible: two case reports. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81(1):103-109.
- Orstavik D. Time-course and risk analyses of the development and healing of chronic apical periodontitis in man. International Endodontic Journal. 1996;29(3):150-155.
- Orstavik D, Pitt Ford TR. Essential Endodontology: Prevention and Treatment of Apical Periodontitis. Malden, MA: Blackwell Science; 1998.
- Pecora G, De Leonardis D, Ibrahim N, Bovi M, Cornelini R. The use of calcium sulphate in the surgical treatment of a ‘through and through’ periradicular lesion. Int Endod J. 2001;34(3):189.
- Pellegrino ED. Patient autonomy and the physician’s ethics. Annals of Royal College of Physicians and Surgeons of Canada. 1994;27(3):171-173.
- Peters LB, Wesselink PR, Moorer WR. The fate and the role of bacteria left in root dentinal tubules. Int Endod J. 1995;28(2):95-99.
- Priebe WA, Lazansky JP, Wuehrmann AH. The value of the roentgenographic film in the differential diagnosis of periapical lesions. Oral Surg Oral Med Oral Pathol. 1954;7(9):979-983.
- Rahbaran S, Gilthorpe MS, Harrison SD, Gulabivala K. Comparison of clinical outcome of periapical surgery in endodontic and oral surgery units of a teaching dental hospital: A retrospective study. Oral Surg Oral Med Oral Pathol. 2001;91(6):700-709.
- Ricucci D, Mannocci F, Pitt Ford TR. A study of periapical lesions correlating the presence of a radiopaque lamina with histological findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(3):389-394.
- Ricucci D, Siqueira JF Jr. Fate of the tissue in lateral canals and apical ramifications in response to pathologic conditions and treatment procedures. J Endod. 2010;36(1):1-15.
- Ricucci D, Siqueira JF Jr, Bate AL, Pitt Ford TR. Histologic investigation of root canal-treated teeth with apical periodontitis: a retrospective study from twenty-four patients. J Endod.
2009;35(4):493-502. - Rud J, Andreasen JO, Jensen JE. A follow-up study of 1,000 cases treated by endodontic surgery. Int J Oral Surg. 1972;1(4):215-228.
- Salehrabi R, Rotstein I. Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. J Endod. 2004;30(12):846-850.
- Siqueira JF Jr, Rôças IN. Polymerase chain reaction-based analysis of microorganisms associated with failed endodontic treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97(1):85-94.
- Siqueira JF Jr, Rôças IN, Lopes HP. Patterns of microbial colonization in primary root canal infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93(2):174-178.
- Sjogren U, Hagglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod. 1990;16(10):498-504.
- Strindberg LZ. The dependence of the results of pulp therapy on certain factors – an analytical study based on radiographic and clinical follow-up examinations. Acta Odontol Scand. 1956;14(suppl 21): 1-174.
- Sundqvist G, Figdor D, Persson S, Sjögren U. Microbiologic analysis of teeth with failed endodontic treatment and the outcome of conservative re-treatment. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod. 1998;85(1):86-93. - von Arx T, Kurt B. Root-end cavity preparation after apicoectomy using a new type of sonic and diamond-surfaced retrotip: a 1-year follow-up study. J Oral Maxillofac Surg. 1999;57(6):656-661.
- Wang Q, Cheung GS, Ng RP. Survival of surgical endodontic treatment performed in a dental teaching hospital: a cohort study. Int Endod J. 2004;37(11):764-775
- World Health Organization. Application of the International Classification of Diseases to Dentistry and Stomatology. 3rd ed. Geneva: World Health Organization; 1995: 66-67.
- World Health Organization. Declaration of Helsinki. British Medical Journal. 1996;313(7070):1448-1449.
- Yu VS, Messer HH, Yee R, Shen L. Incidence and impact of painful exacerbations in a cohort with post-treatment persistent endodontic lesions. J Endod. 2012;38(1):41-46.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..